THE THE ROLE OF NUTRITIONAL STATUS ON HEMOGLOBIN LEVELS IN ADOLESCENTS
DOI:
https://doi.org/10.36720/nhjk.v13i1.637Keywords:
Anemia, Anemia, Hemoglobin, Hemoglobin, Body Mass Index, Body Mass Index, Adolescents, AdolescentsAbstract
Background: Adolescents were one of the strong foundations for the future of the nation because of their role in development and progress of the country. Healthy physical and psychological conditions will form a strong and resilient adolescent character which is affected by adequate nutritional intake. So that if nutrients are not sufficient, it can cause disturbances in metabolic processes. Inadequate intake of nutrients such as protein and iron will aggravate the occurrence of anemia and lead to malnutrition. Indirectly, nutritional status will also affect the occurrence of anemia.
Objectives: This study was to examine the relationship between nutritional status and adolescent hemoglobin levels.
Methods: This study was an analytic study with Cross Sectional approach. Respondents were 46 students of SMP PGRI 01 Bantur in Malang regency conducted in August 2023. Independent variable was nutritional status using weight, height and Body mass index (BMI) and dependent variable was anemia using hemoglobin level. BMI was calculated using formula weight divided by height square. The analysis used both univariate and bivariate analysis. Bivariate analyzed using Spearman rank correlation test.
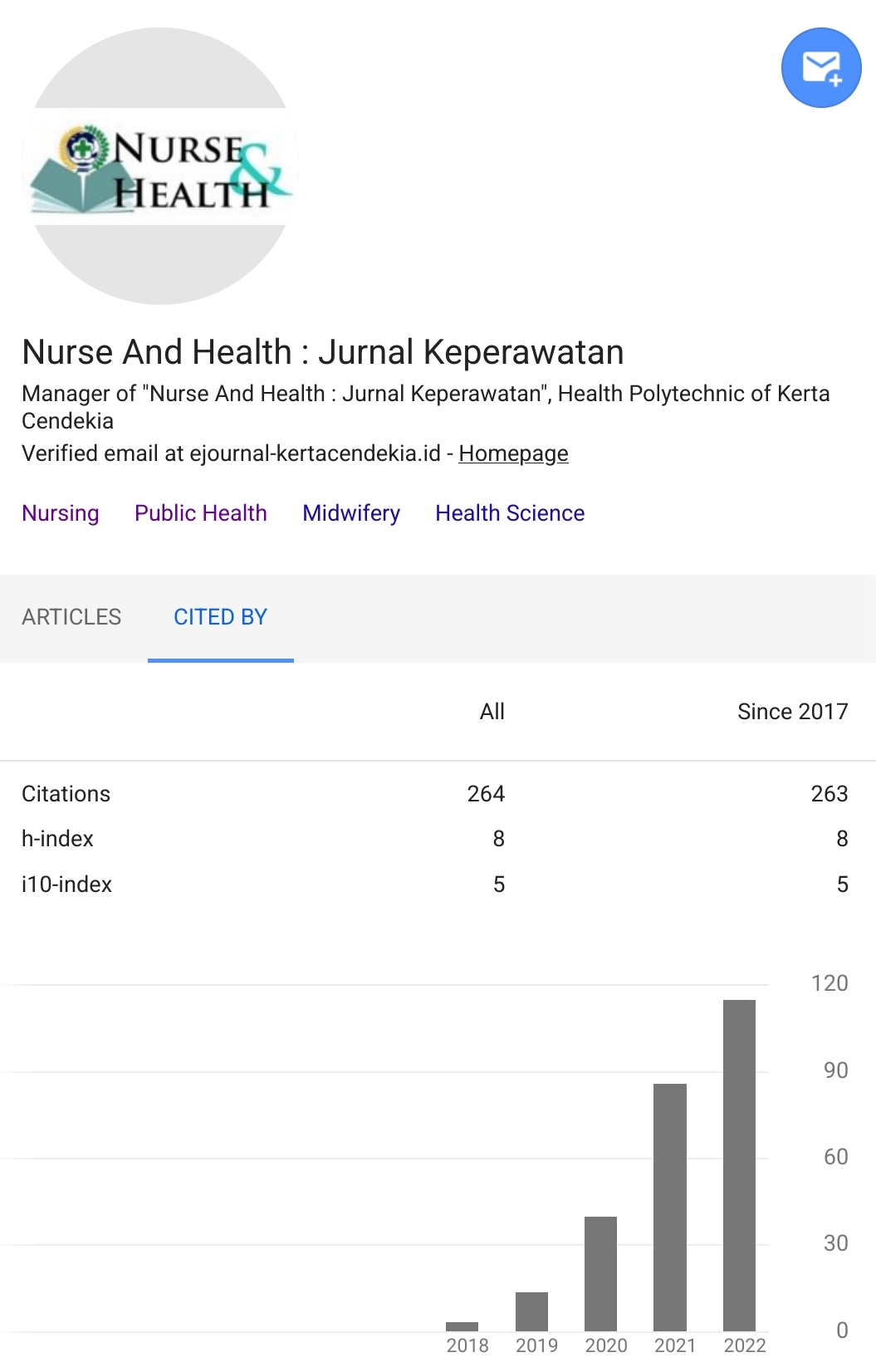
Results: Results showed 76,1% adolescents classified normal nutritional, 19,6% overweight and 2,2% underweight and obese. The hemoglobin level, 86,9% normal and 13,1% anemia. Based on the results of statistical tests using rank spearman test, the p value = 0.044 less than 0,05. It means there was a significant correlation between nutritional status and anemia.
Conclusion: There is a relationship between nutritional status with Hb levels in adolescents. Enrichment of nutritional intake will give big impact on nutritional and anemia status among adolescents.
Downloads
References
Asrullah, M., Hositanisita, H., L’Hoir, M., Muslimatun, S., JM Feskens, E., & Melse-Boonstra, A. (2023). Intra-uterine exposure to lower maternal haemoglobin concentration is associated with impaired cognitive function in stunted adolescents: results from a 17-year longitudinal cohort study in Indonesia. International Journal of Food Sciences and Nutrition, 74(8), 826–835. https://doi.org/10.1080/09637486.2023.2267792
Cairo, R. C. de A., Silva, L. R., Bustani, N. C., & Marques, C. D. F. (2014). Anemia por deficiencia de hierro en adolescentes; una revision de la literatura. Nutricion Hospitalaria, 29(6), 1240–1249. https://doi.org/10.3305/nh.2014.29.6.7245
Camaschella C. (2019). Iron deficiency. Blood, 133(1), 30-39. https://doi.org/doi: 10.1182/blood-2018-05-815944.
Das JK, Salam RA, Thornburg KL, Prentice AM, Campisi S, Lassi ZS, Koletzko B, B. Z. (2017). Nutrition in adolescents: physiology, metabolism, and nutritional needs. Ann N Y Acad Sci., 1393(1), 21–33. https://doi.org/doi: 10.1111/nyas.13330.
De Andrade Cairo RC, Rodrigues Silva L, Carneiro Bustani N, F. M. C. (2014). Iron deficiency anemia in adolescents; a literature review. Nutr Hosp., 29(6), 1240–1249. https://doi.org/doi: 10.3305/nh.2014.29.6.7245.
Deivita Y, Syafruddin S, Andi Nilawati U, Aminuddin A, Burhanuddin B, Z. Z. (2021). Overview of Anemia; risk factors and solution offering. Gac Sanit., 35(2), S235-S241. https://doi.org/doi: 10.1016/j.gaceta.2021.07.034.
Ghose B, Yaya S, T. S. (2016). Anemia Status in Relation to Body Mass Index Among Women of Childbearing Age in Bangladesh. Asia Pacific Journal of Public Health, 28(7), 611–619. https://doi.org/doi:10.1177/1010539516660374
Juffrie M, Helmyati S, H. M. (2020). Nutritional anemia in Indonesia children and adolescents: Diagnostic reliability for appropriate management. Asia Pac J Clin Nutr., 29(1), S18–S31. https://doi.org/doi: 10.6133/apjcn.202012_29(S1).03.
Kemenkes. (2022). Remaja Bebas Anemia: Konsentrasi Belajar Meningkat, Bebas Prestasi. Retrieved from Kementerian Kesehatan Republik Indonesia website: https://ayosehat.kemkes.go.id/remaja-bebas-anemia-konsentrasi-belajar-meningkat-bebas-prestasi
Khan A, Chawla RK, Guo M, W. C. (2019). Risk factors associated with anaemia among adolescent girls: a cross sectional study in District Peshawar, Pakistan. J Pak Med Assoc., 69(11), 1591–1595. https://doi.org/doi: 10.5455/JPMA.295006
Kundu S, Alam SS, Mia MA, Hossan T, Hider P, Khalil MI, Musa KI, I. M. (2023). Prevalence of Anemia among Children and Adolescents of Bangladesh: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health., 20(3), 1786. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36767153/
Leung AKC, Lam JM, Wong AHC, Hon KL, L. X. (2024). Iron Deficiency Anemia: An Updated Review. Curr Pediatr Rev., 20(3), 339–356. https://doi.org/10.2174/1573396320666230727102042.
Lopez A, Cacoub P, Macdougall IC, P.-B. L. (2016). Iron deficiency anaemia. Lancet., 387(10021), 907–916. https://doi.org/doi: 10.1016/S0140-6736(15)60865-0.
Ma J, Huang J, Zeng C, Zhong X, Zhang W, Zhang B, L. Y. (2023). Dietary Patterns and Association with Anemia in Children Aged 9-16 Years in Guangzhou, China: A Cross-Sectional Study. Nutrients., 15(19), 4133. https://doi.org/doi: 10.3390/nu15194133.
Cite this article as: Kusbandiyah, J., et al. (2024). The Role of Nutritional Status on Hemoglobin Levels in Adolescents. Nurse and Health: Jurnal Keperawatan, 13 (1), 78-83. https://doi.org/10.36720/nhjk.v13i1.637
Mukherjee SB. (2016). Growth, Nutritional status and Anemia in Indian Adolescents. Indian Pediatr, 53(10), 905-906. https://doi.org/doi: 10.1007/s13312-016-0956-3.
Norris SA, Frongillo EA, Black MM, Dong Y, Fall C, Lampl M, Liese AD, Naguib M, Prentice A, Rochat T, Stephensen CB, Tinago CB, Ward KA, Wrottesley SV, P. G. (2022). Nutrition in adolescent growth and development. Lancet., 399(10320), 172-184. https://doi.org/doi: 10.1016/S0140-6736(21)01590-7.
Samson KLI, Fischer JAJ, R. M. (2022). Iron Status, Anemia, and Iron Interventions and Their Associations with Cognitive and Academic Performance in Adolescents: A Systematic Review. Nutrients., 14(1), 224. https://doi.org/doi: 10.3390/nu14010224.
Ukoha OM, Emodi IJ, Ikefuna AN, Obidike EO, Izuka MO, E. C. (2020). Comparative study of nutritional status of children and adolescents with sickle cell anemia in Enugu, Southeast Nigeria. Niger J Clin Pract., 23(8), 1079-1086. https://doi.org/doi: 10.4103/njcp.njcp_476_19
Weyand AC, Chaitoff A, Freed GL, Sholzberg M, Choi SW, M. P. (2023). Prevalence of Iron Deficiency and Iron-Deficiency Anemia in US Females Aged 12-21 Years, 2003-2020. JAMA, 329(24), 2191-2193. https://doi.org/doi: 10.1001/jama.2023.8020.
WHO. (2023). Adolescent and young adult health. Retrieved from WHO website: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions
Downloads
Published
How to Cite
Issue
Section
Citation Check
License
Authors who publish with Nurse and Health: Jurnal Keperawatan agree to the following terms:
- Authors retain copyright licensed under a Creative Commons Attribution-NonCommercial 4.0 (CC BY-NC 4.0), which allows others to remix, tweak, and build upon the authors' work non-commercially, and although the others' new works must also acknowledge the authors and be non-commercial, they don't have to license their derivative works on the same terms.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). Authors can archive pre-print and post-print or publisher's version/PDF.